Abstract
Background: Inotuzumab ozogamicin (INO) is a humanized, anti-CD22 antibody conjugated to calicheamicin with FDA approval for treatment of adults with relapsed or refractory (r/r) B-acute lymphoblastic leukemia (B-ALL). While it is associated with favorable complete remission rates in r/r B-ALL patients (pts), hepatotoxicity both during treatment and with subsequent hematopoietic cell transplantation (HCT) remains a challenge. In general, venoocclusive disease (VOD) during HCT in pediatric pts is estimated at 10-20%. Following treatment with INO, however, up to 52% of pts undergoing HCT have been reported to develop VOD, of which 18% of cases were fatal (Bhojwani et al. 2019). Here we report our institutional HCT experience in pediatric pts with r/r B-ALL who underwent HCT following INO reinduction and our strategy of using defibrotide prophylaxis to reduce the risk of VOD.
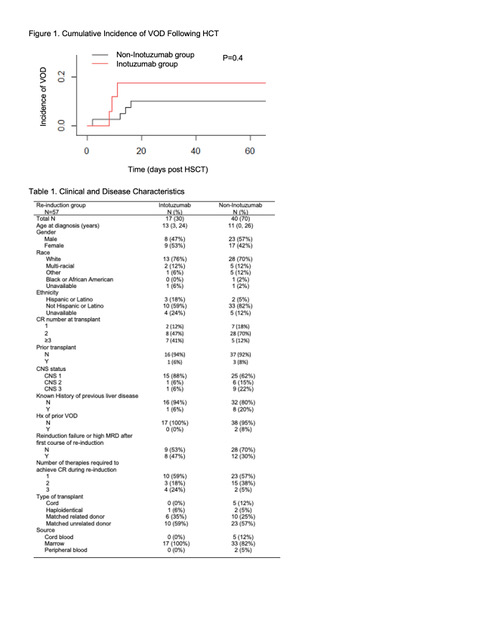
Methods: A retrospective chart review was conducted for pts with r/r B-ALL who underwent HCT at our institution from December 2015 to January 2021. Clinical characteristics, laboratory parameters, and radiographic evaluations were reviewed. Patients who received ≥1 course of INO during reinduction were included in the INO group. Development of VOD was defined as a clinical diagnosis of VOD post-HCT based on either the Baltimore, Seattle, or European Society for Blood and Marrow Transplantation (EBMT) diagnostic criteria.Clinical characteristics were summarized. Time to VOD, graft versus host disease (GVHD), non-relapse mortality (NRM), and relapse were estimated under the competing risk setting, in which death without the event of interest was considered to be an absorbing competing risk.
Results: Fifty-seven patients with relapsed or refractory B-ALL were transplanted between December 2015 and January 2021. Seventeen (30%) received at least 1 course (3 doses) of INO as part of their pre-HCT reinduction regimen. Fifty-five of 57 pts (97%), including all pts in the INO-group received a myeloablative regimen (51 total body irradiation/cyclophosphamide-based, 4 busulfan-based). Two patients in the non-INO group received a reduced-intensity regimen. Median time from last dose of INO to HCT (Day 0) was 34 days (range 24-71 days). Median number of INO doses received was 6 (range 3-9). Four patients had been transplanted previously, 1 in the INO group and 3 in the non-INO group. Two of these patients developed VOD during their current HCT, both from the non-INO group. Pts receiving INO were more likely to be transplanted in CR3 or higher, and to have required 3 regimens in reinduction to achieve that CR. Median follow-up was 20 months.
Rates of VOD were similar between the INO (3 of 17, 18%) and non-INO (4 of 40, 10%) groups (p=0.4, Figure 1). All cases were severe or very severe by EBMT criteria. There was no VOD-related mortality in either group. Defibrotide prophylaxis was used in 82% (14 of 17) of pts in the INO group. Of the 3 patients in the INO group who developed VOD, 2 received defibrotide prophylaxis and 1 did not. Reasons to defer defibrotide prophylaxis included increased risk of CNS bleeding and provider preference. Defibrotide prophylaxis was used in 15% of pts in the non-INO group (6 of 40). In the non-INO group, 1 of 4 patients who developed VOD had received defibrotide prophylaxis. All pts received vitamin E and ursodiol per institutional practice.
There were no treatment-related deaths in the INO group and no statistically significant differences were detected in (NRM) (0% vs 10%, p=0.25), median time to engraftment (24 vs 26.5 days, p=0.1), or GVHD (24% vs 55%, p=0.1) in the INO vs non-INO groups.
Conclusions: HCT was well tolerated with low rates of VOD and NRM in pediatric pts following reinduction with INO. The results of ongoing prospective studies will provide further insight into the role of INO for reinduction of r/r B-ALL. In our cohort, rates of VOD were similar between pts who had and had not previously received INO, with the majority of pts in the INO group receiving defibrotide prophylaxis during HCT, suggesting that inotuzumab ozogamicin reinduction may safely be used with this approach.
Margossian: Cue Biopharma: Current Employment. Silverman: Takeda, Servier, Syndax, Jazz Pharmaceuticals: Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees. Neuberg: Pharmacyclics: Research Funding; Madrigal Pharmaceuticals: Other: Stock ownership.
This study evaluates the safety of transplant following inotuzumab ozogamicin re-induction for children with B lymphoblastic leukemia.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal